Nurses need physiology autonomic dysreflexia – Nurses play a vital role in the assessment, management, and prevention of autonomic dysreflexia, a potentially life-threatening condition that can affect individuals with spinal cord injuries. Understanding the physiology of autonomic dysreflexia is essential for nurses to provide effective and timely care.
This article provides an overview of the physiological mechanisms, signs and symptoms, and potential complications of autonomic dysreflexia. It also discusses the nursing assessment process, interventions, and the importance of patient education and support. Additionally, the article emphasizes the significance of interdisciplinary collaboration and evidence-based guidelines in managing autonomic dysreflexia.
Definition and Overview of Physiology Autonomic Dysreflexia: Nurses Need Physiology Autonomic Dysreflexia
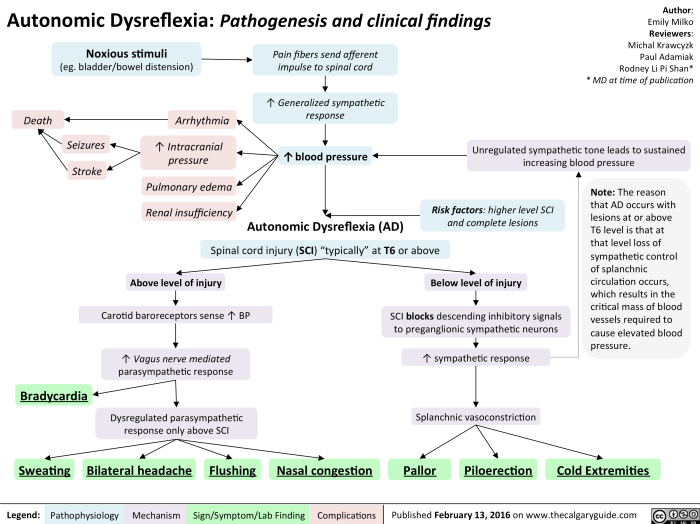
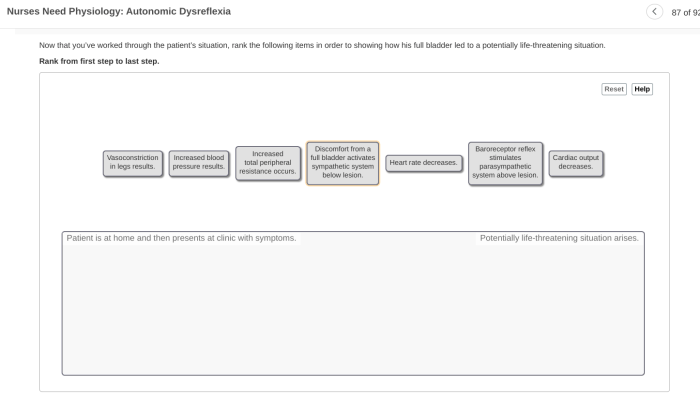
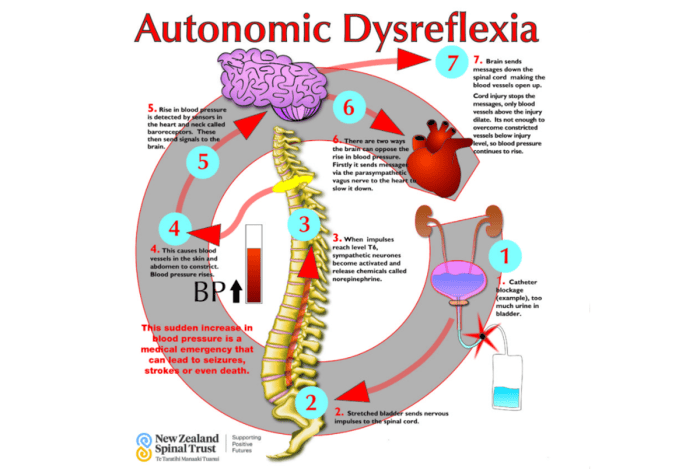
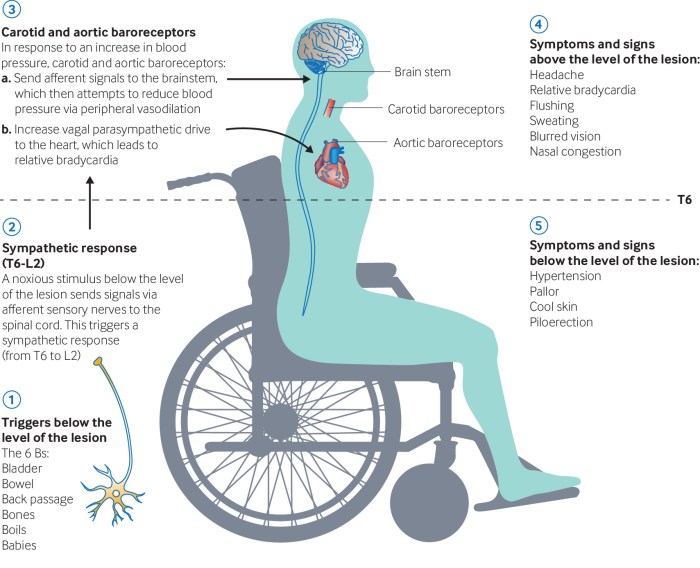
Autonomic dysreflexia (AD) is a life-threatening condition that can occur in individuals with spinal cord injuries (SCI) at or above the T6 level. It is caused by an exaggerated sympathetic response to noxious stimuli below the level of the SCI, leading to a sudden and potentially dangerous increase in blood pressure.
Physiological Mechanisms of Autonomic Dysreflexia, Nurses need physiology autonomic dysreflexia
In individuals with SCI, the descending inhibitory pathways from the brain to the sympathetic nervous system are disrupted. This results in an overactivity of the sympathetic nervous system, which can be triggered by various stimuli, including:
- Bladder or bowel distension
- Skin irritation or injury
- Urethral or vaginal stimulation
- Cold or heat exposure
When triggered, the sympathetic nervous system causes:
- Vasoconstriction below the level of the SCI, leading to increased blood pressure
- Bradycardia (slowed heart rate)
- Sweating above the level of the SCI
- Dilated pupils
- Headache
- Nasal congestion
If left untreated, AD can lead to severe complications, including stroke, seizures, and even death.
Nursing Assessment and Management of Autonomic Dysreflexia
Nurses play a critical role in assessing and managing AD in individuals with SCI. The nursing assessment process includes:
- Thorough history taking to identify potential triggers
- Physical examination to monitor vital signs and assess for signs and symptoms of AD
- Regular bladder and bowel management
Nursing interventions for managing AD include:
- Identifying and eliminating the triggering stimulus
- Administering antihypertensive medications as prescribed
- Applying a sitz bath or cold pack to the lower extremities
- Encouraging deep breathing and relaxation techniques
Patient education and support are essential for preventing and managing AD. Nurses should educate patients about:
- The signs and symptoms of AD
- The importance of avoiding triggers
- Proper bladder and bowel management techniques
- The importance of seeking immediate medical attention if AD occurs
Interdisciplinary Collaboration in Autonomic Dysreflexia Care
Managing AD effectively requires a team approach involving various healthcare professionals, including:
- Nurses
- Physicians
- Physical therapists
- Occupational therapists
- Urologists
Interdisciplinary communication and coordination are crucial for providing comprehensive care. The team should work together to:
- Develop an individualized care plan
- Identify and address potential triggers
- Monitor and manage symptoms
- Educate patients and their families
Involving patients and their families in the decision-making process is essential for ensuring their understanding and adherence to the care plan.
Case Studies and Best Practices in Autonomic Dysreflexia Management
Case studies can illustrate the successful management of AD. One example is a patient with a T7 SCI who experienced AD due to a distended bladder. The nurse identified the trigger, emptied the bladder, and administered antihypertensive medication. The patient’s blood pressure returned to normal, and the AD symptoms resolved.
Best practices for preventing and treating AD include:
- Regular bladder and bowel management
- Avoiding triggers
- Prompt treatment of infections
- Patient education and support
Evidence-based guidelines for managing AD are available from organizations such as the American Spinal Injury Association and the National Institute on Disability, Independent Living, and Rehabilitation Research.
Quick FAQs
What is autonomic dysreflexia?
Autonomic dysreflexia is a condition that can occur in individuals with spinal cord injuries above the T6 level. It is characterized by a sudden and severe increase in blood pressure, which can lead to serious complications such as stroke, seizures, and even death.
What are the signs and symptoms of autonomic dysreflexia?
The signs and symptoms of autonomic dysreflexia include a sudden increase in blood pressure, headache, sweating, flushing, and goosebumps. Individuals may also experience nausea, vomiting, and blurred vision.
What is the nursing role in managing autonomic dysreflexia?
Nurses play a vital role in managing autonomic dysreflexia. They are responsible for assessing for signs and symptoms, implementing interventions to prevent and treat the condition, and educating patients and their families about autonomic dysreflexia.